WHAT IS IT AND HOW TO CURE THE HERNIATED DISC
In a man’s life there are few certainties, and one of these is that sooner or later he will suffer from back pain.
 One of the most common causes of back pain is certainly represented by a slipped disc. The symptomatic lumbar disc herniation is a degenerative disease of the intervertebral disc that manifests with a clinical picture that is characterized by back pain, sciatica or radiculopathy compression and crucial limitation or loss of function. Natural history studies indicate that hernias of the intervertebral disc are resorbed often wholly or in part and that the symptomatology associated with them frequently regresses with conservative treatments. Herniated lumbar discs are detected with diagnostic imaging with high frequency in people of all asymptomatic backgrounds. Therefore, the herniated disc is a dynamic phenomenon, as well as a relatively common condition and favorable prognosis in most cases. (Istituto Superiore Sanità, Guidelines disc herniation).
One of the most common causes of back pain is certainly represented by a slipped disc. The symptomatic lumbar disc herniation is a degenerative disease of the intervertebral disc that manifests with a clinical picture that is characterized by back pain, sciatica or radiculopathy compression and crucial limitation or loss of function. Natural history studies indicate that hernias of the intervertebral disc are resorbed often wholly or in part and that the symptomatology associated with them frequently regresses with conservative treatments. Herniated lumbar discs are detected with diagnostic imaging with high frequency in people of all asymptomatic backgrounds. Therefore, the herniated disc is a dynamic phenomenon, as well as a relatively common condition and favorable prognosis in most cases. (Istituto Superiore Sanità, Guidelines disc herniation).
What is a herniated disc?
 To understand what a herniated disc is, you must first know the anatomy of the spinal column. The spine is made up of 32-33 vertebrae (7 cervical, 12 thoracic and 5 lumbar, 5 sacral and 3-4 coccygeal). Each vertebra is numbered with an increasing number from top to bottom, C1-C2-C3 … C7-T1-T2-T3 … T12-L1-L2-L3-L4-L5-S1 … the last lumbar vertebra, called L5, is placed above the first vertebra of the sacrum, named S1. Between a vertebra and the other are interposed soft pads called intervertebral discs, which are appointed and leads through the number and location of the vertebra above and below. For example, the C4-C5 disc is the disc between the fourth and fifth cervical vertebra, while the disc between the fourth and fifth lumbar vertebrae is called disc L4-L5.
To understand what a herniated disc is, you must first know the anatomy of the spinal column. The spine is made up of 32-33 vertebrae (7 cervical, 12 thoracic and 5 lumbar, 5 sacral and 3-4 coccygeal). Each vertebra is numbered with an increasing number from top to bottom, C1-C2-C3 … C7-T1-T2-T3 … T12-L1-L2-L3-L4-L5-S1 … the last lumbar vertebra, called L5, is placed above the first vertebra of the sacrum, named S1. Between a vertebra and the other are interposed soft pads called intervertebral discs, which are appointed and leads through the number and location of the vertebra above and below. For example, the C4-C5 disc is the disc between the fourth and fifth cervical vertebra, while the disc between the fourth and fifth lumbar vertebrae is called disc L4-L5.
 In most cases, the disc herniation occurs in the lumbar region (95% in the L4-L5 and L5-S1), followed by cervical region (many times C5-C6, C6-C7), and then by only 0.15% / 4.0% of cases in the thoracic region. The thoracic discs are, in fact, very stable and hernias in this region are quite rare.
In most cases, the disc herniation occurs in the lumbar region (95% in the L4-L5 and L5-S1), followed by cervical region (many times C5-C6, C6-C7), and then by only 0.15% / 4.0% of cases in the thoracic region. The thoracic discs are, in fact, very stable and hernias in this region are quite rare.
The intervertebral discs have a thickness ranging from 6-7 mm to 10-12 mm and a diameter equal to that of the adjacent vertebrae and act as shock absorbers between the vertebras. When we bend, the disc is changed so as to facilitate the movement of the spine. When we skip, the disk allows to mitigate the impact on the vertebrae. This deformability of the disc is related to its structure: a central part soft and rich in water, called the nucleus pulposus, and a peripheral part consisting of more resistant and fibrous material, called the annulus fibrous.
For reasons not entirely clear (Individual predisposition overload? posture? Smoke? …), the outer part of the fiber can lose its ability to hold a belt as the nucleus pulposus. This determines the leakage of the nucleus with the formation of disc herniation.
 Many times the fibrous ring though torn is not broken and the disc remains intact although distorted or warped: this is called a disc protrusion or bulging. However, when the fibrous ring is broken, it is called a herniated disc. In this case, the content of the gelatinous content of the disc protrudes to move into the spinal canal, sometimes directly pressing directly against the nerve roots.
Many times the fibrous ring though torn is not broken and the disc remains intact although distorted or warped: this is called a disc protrusion or bulging. However, when the fibrous ring is broken, it is called a herniated disc. In this case, the content of the gelatinous content of the disc protrudes to move into the spinal canal, sometimes directly pressing directly against the nerve roots.
If you want to be very precise you should avoid talking about herniated discs in many cases. The proper name common to all the deformations of the disc should be disc protrusion. In turn, the protrusion is distinct in harmonic or circumferential protrusion (bulging in English), when the disk is expanded in its entire circumference (like a flat tire); and when the focal disc protrusion presents with a deformation in a single point. The latter condition is commonly called herniated discs.
In common parlance and even when the medical professionals speak of protrusions, there is a point when the deformation is a very small hernia, then when the deformation is a slightly larger hernia, and when the deformation is an even larger massive hernia even the doctor is surprised at the size of the hernia! Actually the term hernia should define only those conditions in which the nucleus pulposus wants to escape from the hard disc’s lacerandone fibers (third picture above).
This explains the confusion that sometimes the terms generate … “I thought it was a hernia but it was a protrusion instead” … … “Lucky you, I was diagnosed with a protrusion but the professor told me that it was a hernia instead!” … in fact our two patients have both a protrusion also called hernia, or much better and more clearly, have a deformation of the intervertebral disc.
 Any deformation of the disc can lead to inflammation and pain, whether it is small, very small or very voluminous. Often more than the size of the deformation of the disk affects the venue; it is the classic example of the intraforaminal (herniated disc). As the nerve exits the vertebral canal, a kind of protective tube placed around the spinal cord and nerve roots to perform a protection action, through a relatively small hole with the boney walls, the presence of even a small compression here easily determines major pain. The same deformation (protrusion or herniation, if you prefer) at another point might even go unnoticed without showing any symptoms.
Any deformation of the disc can lead to inflammation and pain, whether it is small, very small or very voluminous. Often more than the size of the deformation of the disk affects the venue; it is the classic example of the intraforaminal (herniated disc). As the nerve exits the vertebral canal, a kind of protective tube placed around the spinal cord and nerve roots to perform a protection action, through a relatively small hole with the boney walls, the presence of even a small compression here easily determines major pain. The same deformation (protrusion or herniation, if you prefer) at another point might even go unnoticed without showing any symptoms.
To simplify this site will use the term hernia is understood in the usual sense.
Why do I have pain?
The lacerationsof the discdetermines therelease of chemical mediatorsof inflammationthat can causesevere paineven in the absenceof adirect compressionof the nerve roots: this is radiculitischemistry that is an inflammatory processinvolvingthe nerve rootsat thepointin whichtheyprotrude from thespine.
The nerve is inflamed at its origin, but the pain you may feel at any point where the nerve goes. The region suffering – the foot, arm or leg – can be perfectly healthy, but the nerve communicates to the brain information that is incorrect because the transmission cable represented by the same nerve transmits the data in an unusual way. The pain is at the bottom but the cause of the pain is in the back. Some patients have pain associated with back or neck, while others are only suffering at the periphery of the leg or arm. This belongs to the characteristics of each individual compression and, above all, the number and quality of nerve fibers involved by inflammation.
Inflammation is the cause of the pain from the herniated disc(s): the nerve hurts when it is inflamed, or when it is compressed. A compressed nerve, but not inflamed by a sense of electric current along its course, just as when you strike your elbow on the edge of something. Certainly, a nerve can be both inflamed and compressed and in this case the pain is more intense.
This explains the use of anti-inflammatory drugs to treat pain caused by herniated discs and protrusions, but explains better why it is possible to have a herniated disc and not experience pain. In fact, many people have disc protrusion or hernias of the column without ever having felt pain.
On this basis, we can now understand why there is today a much more conservative approach, i.e., non-surgical, to herniated discs
FREQUENCY
Disc herniations occur most often between the ages of 30 and 50 years, when the core is still well hydrated and gelatinous. With age the nucleus pulposus changes, it dehydrates gradually and the risk of hernia formation is reduced. The prevalence over the lifetime of lumbar disc herniation has been estimated as 1-3% in Western countries. In 1999 the ISTAT survey on the health status in Italy indicates that 8.2% of the population has been reported to be suffering from “low back pain” (7.3% males and 9.3% females).
Natural history of disk herniation
The symptoms caused by the hernia may resolve spontaneously or with conservative treatment: a number of studies of diagnostic imaging have shown that in a high proportion of cases, the herniated lumbar discs subside completely or in large part.
The improvement is rapid within the first three months and is attributable to mechanisms of cellular resorption mediated by cytokines without fibroblastic reaction. Therefore, the herniated disc is a dynamic phenomenon, as well as a relatively common condition and favorable prognosis in most cases. The 95% of patients with disabling back pain are able to return to work within three months after the onset of symptoms without being subjected to surgery.
Rare are the disc hernias which cause extensive compression, usually considered as a clear indication for surgical intervention. These lesions often regress spontaneously or better from a clinical perspective with conservative treatments: the probabilities of absorption increases with the size of the hernia and the extent of migration from the disc space. Even the neurological deficits caused by lumbar disc herniation (with the exception of cauda equina syndrome and progressive loss of motor function) would be a favorable natural history.
Saal JA. Natural history and non-operative treatment of lumbar disc herniation. Spine1996; 21 (24 Suppl): 2S-9S.
Symptoms
Patients may complain of pain of varying intensity, tingling or a burning sensation. The touch or pain can be reduced or absent, and sometimes can present with a deficit of strength. The location of the symptoms are related to the location of the protrusion or herniation.
Lumbar disc herniation
The symptoms manifest themselves in the back in the lumbar region, buttocks, thighs, and may radiate from the foot up to the toes. The sciatic nerve is the nerve most frequently affected (pain in the leg, back, ankle or toes), more rarely femoral nerves (thigh pain, front, extending to the knee).
Cervical Herniation
Symptoms can affect the back of the head, neck, shoulder blade, shoulder, arm and hand.
RED LIGHTS
 The history and clinical examination of the patient with back pain and/or radicular pain must be directed to identify cases in which the symptoms can be caused by systemic diseases, inflammatory, neoplastic or infectious disease involving the spine. In addition patients who have lower back pain, radiated or not, the so-called red flags must pay close attention to:
The history and clinical examination of the patient with back pain and/or radicular pain must be directed to identify cases in which the symptoms can be caused by systemic diseases, inflammatory, neoplastic or infectious disease involving the spine. In addition patients who have lower back pain, radiated or not, the so-called red flags must pay close attention to:
- Extensive neurological deficit and/or progressive;
2. History of cancer, unexplained weight loss, protracted weakness and fatigue;
3. Fever; - Continuous worsening of pain at rest and at night;
- Recent trauma, prolonged intake of corticosteroids; osteoporosis;
- Clinical picture of cauda equina syndrome with saddle anesthesia in the perineal region, retention or urinary and/or fecal incontinence or bilateral lower limb weakness.
Only a thorough medical examination to rule out diseases allows far more serious herniated disc!
Risk Factors
Are considered risk factors sedentary occupations and physical inactivity, overweight, tall, driving motor vehicles prolonged and constant vibrations, work with high physical effort especially if you are usually composed of manual lifting of loads and pregnancy.
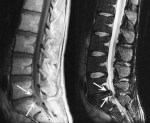
Diagnostics: CT or MRI?
Given the high frequency of spontaneous remission of the clinical or following conservative treatment, in cases where there are no red lights, it is recommended that you wait at least 4-6 weeks after the onset of symptoms before getting medical checkups and diagnostic images. CT and MRI are equivalent in terms of diagnostic accuracy, but MRI has the advantage of not exposing the patient to any radiological risk.
The physicians responsible for the clinical management of the patient must correlate information from the reports of diagnostic imaging with the clinical situation, explaining that the radiological findings of disc protrusion is frequently asymptomatic in the general population.
The use of intravenous contrast agents with CT or MRI is indicated in the diagnosis of lumbar disc hernia in patients already undergoing surgery and only in cases where the study without contrast enhancement has an inconclusive result
The x-ray of the spinal column is not intended as a routine examination in patients with radicular pain, except in cases of suspected spinal fracture or suspected ankylosing spondylitis. We do not recommend carrying out routine electro-physiological tests.
Ozone Therapy
A bit of history
The treatment ofherniasanddisc protrusionwithOzonewas introducedinItalyin 1980, thanks to an orthopedist, Dr. CesareVerga. Then thetreatmentinvolved theinfiltrationof theparavertebral muscleswithavery highvolumeofgas. Thetherapeutic resultsweredisputed by thescientific world, but patients had begun to heal.
In 1984, Dr. Verga presented his findings at a medical conference and did not receive high praise from his colleagues, but patients were continuing to heal using his therapy.
Word of mouth of the healed patients were followed thecuriosityof physicians.
Starting in the 1990’s the first scientific articles began to appear in medical journals with a progressively larger series. Much of the medical world still believed the technique ineffective, nevertheless patients continued to heal.
In early 2000’s ozone therapy with already impressive case studies began to appear, thanks to the tireless work of a neuro-radiologist of Brescia, Dr. Matteo Bonetti, himself motivated by the undisputed authority in the neuro-radiology world, Prof. Marco Leonardi. Over a period of 10 years hundreds of articles are published with adequate standards of data collection and statistical analysis of the results in a scientific world.
The world of health care, while understandably reluctant to accept a therapy based on the use of a gas, gradually became curious. Word of mouth joins sending patients to have the surgeries of ozone therapy by medical colleagues.
The diffusionof ozoneis accompanied by thepresenceof its usebynon-medical personnelandthe emergence ofa number ofissues relatedto the side effectsthat will result in a circularfrom the Minister of HealthSirchiathatsuspendsthe useinItaly. This will be followeda few monthsafter thesuspension of theministerial circularby theLazio Regional Administrative Courtand the fundamentalCircular of theLombardy Region, whichauthorizes itsuse onlyindoctors’ surgeriesandcareby medical personnel.
In those years, by the author of the site, a more through analysis of the side effects related to the administration of mixtures of Oxygen-Ozone for the treatment of hernias and disc protrusions and generally of each treatment infiltrative treatment was developed. They will come out with several articles reporting the causes and the measures to be taken to avoid any major side effects, different techniques are revisited and it is shown in a scientific manner that doses and volumes of Oxygen-Ozone to be within certain parameters to achieve the same resolution of the pathological and the substantial absence of side effects. It is with great personal pleasure that I look, after 7 years from the publication of my first article about side effects; there have been more reports of greater side effects in the group of doctors who identify themselves with the Italian Federation of Ozone Therapy (FIO).
THE TECHNIQUES
Over the years I have followed courses and conferences in Italy as well as abroad with the aim of forming and creating a scientific culture around the world regarding ozone therapy.
Currently, the techniques used for the treatment of herniated discs that involve the following three techniques:
- Para-vertebral
- Intraforaminal with radiological guidance (luminance amplifier, TAC)
- Intradisc
Although in many cases the indications overlap, so it is possible to treat a hernia or protrusion with more than one technique, the medical experts can suggest the best method based on the morphology and location of the hernia based on the symptoms and characteristics of the patient.
Para Vertebral Technique.
Represents the historical technique, the “mother” of all ozone treatments of the vertebral column and spine. No doubt it is the most commonly used method. Relative simplicity, great efficacy, few side effects (with proper technique!), and very few contraindications.
The patient should be placed on a bed with her back facing upwards. Identified the site of the hernia or protrusion you administer a mixture of oxygen-ozone in the muscles on the sides of the spine. The administration is done through very fine needles and, is not particularly painful.
Indications found inmany pathologies of the spine:
- herniated discs
• disc protrusion
• osteoarthritis
• spinal canal stenosis
However, the apparent simplicity of the technique, one must not ignore:
- thorough disinfection
• disposable material
• use of 20 ml syringes, you should not use syringes 50-60 ml for the high risk of inadequate doses of quantitative and potentially dangerous for the patient.
• stay for a few minutes on the couch in the office and remain ambulatoryThe percentages of painful resolution reaches75-80%of positive results.
Technical information
The treatment with a mixture of oxygen-ozone intraforaminal requires the use of an image intensifier or TAC for the precise positioning of the needle tip at the point of exit of the inflamed nerve from the spinal canal. The treatment is carried out after a thorough disinfection of the skin, followed by local anesthesia with ice spray. Rarely is painful for the patient, after about 15-20 minutes, can return to his home.
This technique represents the evolution and refinement of the classic paravertebral injections. Ozone arrives exactly on the nerve roots that are suffering because of the protrusion or herniation. The use of radiological equipment allows to continuously check the accuracy of the method.
The technique is important for several reasons:
1. The fastest resolution of the painful area.
2. The administration of ozone in the immediate vicinity of the nerve that is the spinal ganglion, other anatomical structures involved in the genesis of pain from disc compression.
3. The ability to radio logically treat and documented the spread of Oxygen-Ozone avoiding any complication.
4. The execution of delivering accurate dose even in regions subverted by the presence of scars due to previous surgical procedures (for example in the seat of residual pain post-surgery).
Technical intral-discal
Usually you run 4-5 infiltration at intervals of one to two weeks, or perform an initial infiltration intraforaminale followed by a classic infiltrative para-spinal cycle.
The rates of resolution of the painful reaches 85% of positive results.
The techniqueisless well knownto patientseven though it isthe most representedin the world of scientific literature. It has describedmore than20,000 patients that weretreated with this techniqueover the past10 years,the resultswere the subject of a recentlyso-calledmeta-analysis, that is, a studythat comparesmany studiesamongthem,who describedthe results withtwo simple words: “very impressive! “- really impressive!The results obtained, especially in different types ofherniaorprotrusive repair, are similarto surgery, and unlike the side effectsare much smallerin number andin quality.
It is a typical indication in all forms of protrusion (i.e. with intact annulus fibrosus) with symptoms that do not respond to less invasive treatments. However, there are no absolute contra-indications to the treatment of hernias contained.
The patient does not require anesthesia or sedation. Through a radiological Guide (image intensifier or CT), a needle is inserted into the warped disc and is given a small amount of Oxygen-Ozone that can cause decompression of the disc through a process of dehydration. At the end of treatment in some centers follows, during the release of the needle, administration of ozone in the intraforaminale; in other centers is cortrisone is administered instead to promote, in either case, the anti-inflammatory process dependent on the nerve, a process which is the basis of the resolution of the pain from disc protrusion or hernia.
The rate of painful resolution reaches 85% of positive results.
Surgery
Geographic variability of interventions for lumbar disc herniation reflects the uncertainty regarding the surgical indications. In Italy every year there are about thirty thousand surgeries with a diagnosis of lumbar disc herniation, which corresponds to an average rate in the three year period of 1999-2001 amounting to 5.09 per 10,000. The standard regional rates for age and sex fluctuate widely, from 6.87 to 2.52 per 10,000 in Lombardy in Calabria. So there are some regions in which they do more hernia operations in greater percentage than in other regions.
The cauda equina syndrome from herniated intervertebral disc is an absolute indication for intervention discectomy to be carried out within 24 hours after symptom onset. The appearance of motor deficit worsening in a patient with established diagnosis of lumbar disc herniation requires taking into account the surgery, even if it is an absolute indication.
For elective indications, covering more than 95% of surgical cases, there must be always a correspondence between the symptoms reported by the patient (radiation of pain and paresthesias), the clinical objective (clinical trials and reflexes) and the instrumental diagnostic imaging confirming the level of involvement of the disc.
Ifthiscongruenceis satisfied,it is recommended toconsidersurgeryinthe presence of allthe following criteria:
- duration of symptomsmore than six weeks;
• persistent pain unresponsive to analgesic treatment;
• failure, in the opinion of both the surgeon and the patient, conservative treatments effective properly conducted.It is very important that the patient is involved in the decision-making process and adequately informed about the natural history of the disease and treatment options.
A further element of caution to indicate surgery is represented by the age of the patient, which is an unfavorable prognostic factor of postoperative outcome. The concomitant presence of severe degenerative spine or peripheral neuropathy is a contraindication to intervention of discectomy.
Which surgery?
There is good evidence that the standard discectomy is more effective than conservative treatment for the resolution of the pain but the effect is limited in time and tends to zero to four years after surgery. The effectiveness of micro-discectomy is equal to the standard discectomy. There is insufficient evidence on the effectiveness of automated percutaneous discectomy and interventions with laser or with coblation.
Whereas the effect of discectomy after a long time is comparable to conservative treatments and herniated discs are resorbed healing spontaneously with high frequency, it is essential that the patient be given a full briefing on the natural history of the condition, the better efficacy of time-limited surgical treatment compared with conservative treatment, and the risks related to surgery and therapeutic alternatives.
There is evidence that information improves the prognosis of the patient’s overall condition. The patient must actively participate in the choice of treatment strategy even compared to his lifestyle and preferences.
Surgical Complications
The spine surgery is not exempt from fearful intra and post-operative complications, such as discitis, the damage to the nerve roots, the immediate or late vascular complications and spinal instability.
Overall:
- incidence ofoperative complicationsis equal to 3-6%,
• risk of re-operation is equal to 3-15%,
• risk of mortality at 30 days after surgery varies between 0.5 and 1.5 per 1,000 patients operated on (!)
Spinal instability, characterized by irregular movement between one or more vertebrae that can cause intermittent nerve root compression, is one of the main causes of failed-back syndrome. Incidence progressively increases with subsequent re-operations up to over 60% in patients who underwent multiple revisions.
Herniated discs recurrence after surgery
Retrospective studies based on data from the hospital information system conducted in Finland of patients operated on for lumbar disc herniation estimated cumulative risks of reoperation at nine years equal to 18.9%, and follow-up actions after the first reoperation ten years of operations equal to 25.1%, then we understand that each subsequent reoperation increases the risk of further intervention. Other sources report that the rates of reoperation after lumbar disc surgery vary widely from 3% to 15%.
There is currently no data relating to the Italian hospitals (!).
How many surgeries are performed in Italy and in the world?
International variations have been described as very large rates of surgery for lumbar disc herniation dating back to the 1908’s: from 10 per 100,000 in Britain to more than 100 per 100,000 in the USA.
In the USA, from 1979 to 1990, it was observed there was 33% increase in rates of lumbar spine surgery. The rates increase linearly with the number of neurosurgeons and orthopedic per capita and fluctuate widely between the various federal states.
As part of the Maine Lumbar Spine Study, the relationship between outcome and volume of work performed had been investigated. Unlike what is known for other surgical procedures, it is very interesting to note that treatment outcomes in patients operated on by surgeons in areas with lower intervention rates were significantly better than in patients of the areas with high rates.
In Italy, the average rate of surgical procedures in the 1999-2001 period amounted to 5.09 per 10,000. The standardized rates ranging between 6.87 and 2.52 per 10,000 in Lombardy and Calabria. The temporal variability in the three year period instead was contained; the absolute number of transactions has increased from 28,231 in 1999 to 30,243 in 2001.
With a wider selection of cases which also includes low back pain, sciatica, lumbar spondylosis, spondylolisthesis and canal stenosis as principal diagnosis, the average rate of surgery for lumbar disc herniation is equal to 6.1 per 10,000 in the 1999-2001; the period fluctuated between 8.12 and 3.40 per 10,000 in Lazio and Sardinia.
Geographic variability of herniated disc surgery reflects the uncertainty on the optimal use of procedures as well as the extent of the “medical disagreement” regarding the indications for surgery.
Epidemiological studies suggest that, in the case of surgery of lumbar disc herniation, appropriateness of interventions and postoperative outcomes go hand in hand.
Which technique should I choose?
It is important to have a doctor that you have confidence in. The “pilgrimage” from various doctors to compare the different opinions, while understandable from a rational point of view, they produce only an extreme confusion.
Because many people suffer from back pain or sciatica, it will be easy to find many people, acquaintances and friends who suggest extremely different treatments from each other, “a friend of mine is going healed by Dr. Vattelapesca “,” going by my physiotherapist Dick “,” my cousin instead did the ozone,” ” My father has done the nitrogen “,” I have not done anything, and after three weeks I was better.”
But what should I do?
In the absence of traffic lights, Rossi is a smart choice to start from minimally invasive techniques to finish, in the absence of any response, with more invasive techniques. This approach represents the criterion suggested by the major scientific societies. When you choose a treatment/therapy (conservative or surgical) always ask about the success rate and recurrence, and most importantly, what are the complications (if any) that are associated with the different techniques.
A thorough examination with the appropriate clinical investigations and subsequent evaluation of radiological investigations (recent!). These need to be accompanied by precise information about the different treatment options available and represent the best clinicians that are involved with the procedures and are the best to visit and discuss your options.
ALESSANDRO SICURO